Multiple births in fertility treatment 2019
UK multiple birth statistics for IVF and DI fertility treatment
Published: February 2022
Download the underlying dataset as Excel Worksheet.
Table of contents
- Main points
- History of multiple births in the UK
- Section 1. Multiple births reduced following cross-sector collaborative efforts
- Section 2. Single embryo transfers increased most among young patients
- Section 3. Largest improvements in multiple birth rate among youngest and oldest patients
- Section 4. Multiple embryo transfers put younger patients at greatest risk of multiple birth
- Section 5. Greater risk of multiple births when using donor eggs
- Section 6. Multiple birth rates higher among Black patients
- Section 7. Higher multiple birth rate among younger privately funded patients
- Section 8. Twin births risk premature birth and associated health risks
- Conclusions and next steps
- About our data
Main points
- Multiple births cause increased risk of health problems for patients and their babies, such as late miscarriage, premature delivery, gestational diabetes, still birth and neonatal and maternal death.
- The risk of multiple birth has commonly been higher in IVF patients due to the clinical practice of transferring multiple embryos to the womb.
- The HFEA launched the collaborative ‘One at a time’ campaign in 2007 to reduce high multiple births from IVF in the UK by using incremental decreases in clinic multiple birth targets.
- The average UK multiple birth rate from IVF treatment has decreased from around 28% in the 1990s to 6% in 2019.
- Birth rates from IVF have continued to rise while the multiple births rate has fallen, which may be due in part to improved embryo selection.
- Single embryo transfers increased in use from 13% of IVF cycles in 1991 to 75% in 2019.
- The multiple birth rate has reduced most among patients under 35 (from 27% in 2007 to 6% in 2019) and patients over 44 (from 31% in 2007 to 5% in 2019).
- Single embryo transfers limited multiple births to around 1-3% across all patient ages.
- Highest multiple birth rate among patients aged 35 and under (above 30%) receiving double embryo transfers.
- When donor eggs were used, transferring multiple embryos carried a greater risk of multiple births (around 30% across all ages) from 2015-2019.
- Black patients typically had higher multiple birth rates at around 12% from 2015-2019, compared to 10% across all ethnic groups.
- Privately funded patients aged 37 and under had higher rates of multiple births from 2015-2019 in their first IVF cycle compared to NHS-funded patients.
- About 60% of IVF twin births were preterm (under 37 weeks) compared to 9% of singleton births from 2015-2019.
- We have outlined a number of actions in our next steps section for ourselves, clinics and others in our continued effort to reduce multiple births.
History of multiple births in the UK
For many years multiple pregnancies and births have been the single biggest health risk of fertility treatment for both patients and babies. A multiple pregnancy increases the risk of stillbirth, neonatal death and disability. Compared with singletons, twins are four times more likely to die in pregnancy, seven times more likely to die shortly after birth, ten times more likely to be admitted to a neonatal special care unit and have six times the risk of cerebral palsy. Maternal morbidity and mortality are also increased due to late miscarriage, high blood pressure, pre-eclampsia and haemorrhage 1-4.
Multiple births from IVF are largely a result of transferring more than one embryo to the womb in treatment. In 2003, the HFEA introduced restrictions on triple embryo transfers to reduce multiple births. These restrictions prevented the use of triple embryo transfer in fertility patients under 40 years of age, apart from in exceptional circumstances.
In the early 2000s, the HFEA commissioned a group of fertility and public health experts to report on the risks of multiple births from fertility treatment, culminating in 2006 with the publication of the One child at a time report. The HFEA then ran a consultation on how we could reduce the multiple birth rate in 2007.
The ‘One at a time’ campaign was launched in 2007 and encouraged clinics to transfer one embryo and freeze any remaining embryos for good prognosis IVF patients. The combination of these policies and concerted efforts across the fertility sector led to fewer double embryo transfers, and fewer multiple births as a result.
A consensus statement was signed by the key professional bodies and stakeholders and the HFEA introduced a multiple birth target in 2009 which licensed clinics were expected to meet. Clinics were also required to develop their own multiple births minimisation strategies which are reviewed routinely in inspections (see State of the Sector report).
The collaboration between the HFEA and the sector encouraged the sharing of best practice and developing professional guidance and improved NHS provision was encouraged.
Information was published for patients and professionals about multiple births, including evidence that transferring a single embryo did not negatively impact a patient’s chance of having a baby.
The reduction in multiple births from IVF has been a huge public policy success in relation to the health of patients and babies. This report highlights areas of success in reducing multiple births and points to areas that should be further considered in clinic minimisation strategies.
1. Multiple births reduced following cross-sector collaborative efforts
In the early 1990s, the average UK multiple birth rate from IVF was around 28% (Figure 1). Following the launch of the ‘One at a time’ campaign in 2007, multiple birth rate targets were introduced and the 10% target was reached nationally in 2017. Multiple birth rates have continued to decline and reached 6% in 2019.
Importantly, birth rates have continued to rise while the multiple birth rate has fallen. This may be due in part to increased use of single embryos at day five of development (blastocyst). Blastocyst embryos have been increasingly used in practice in the UK and may have helped to maintain birth rates from single embryo transfer while decreasing multiple birth rates.
IVF average live multiple birth rate, 1991-2019
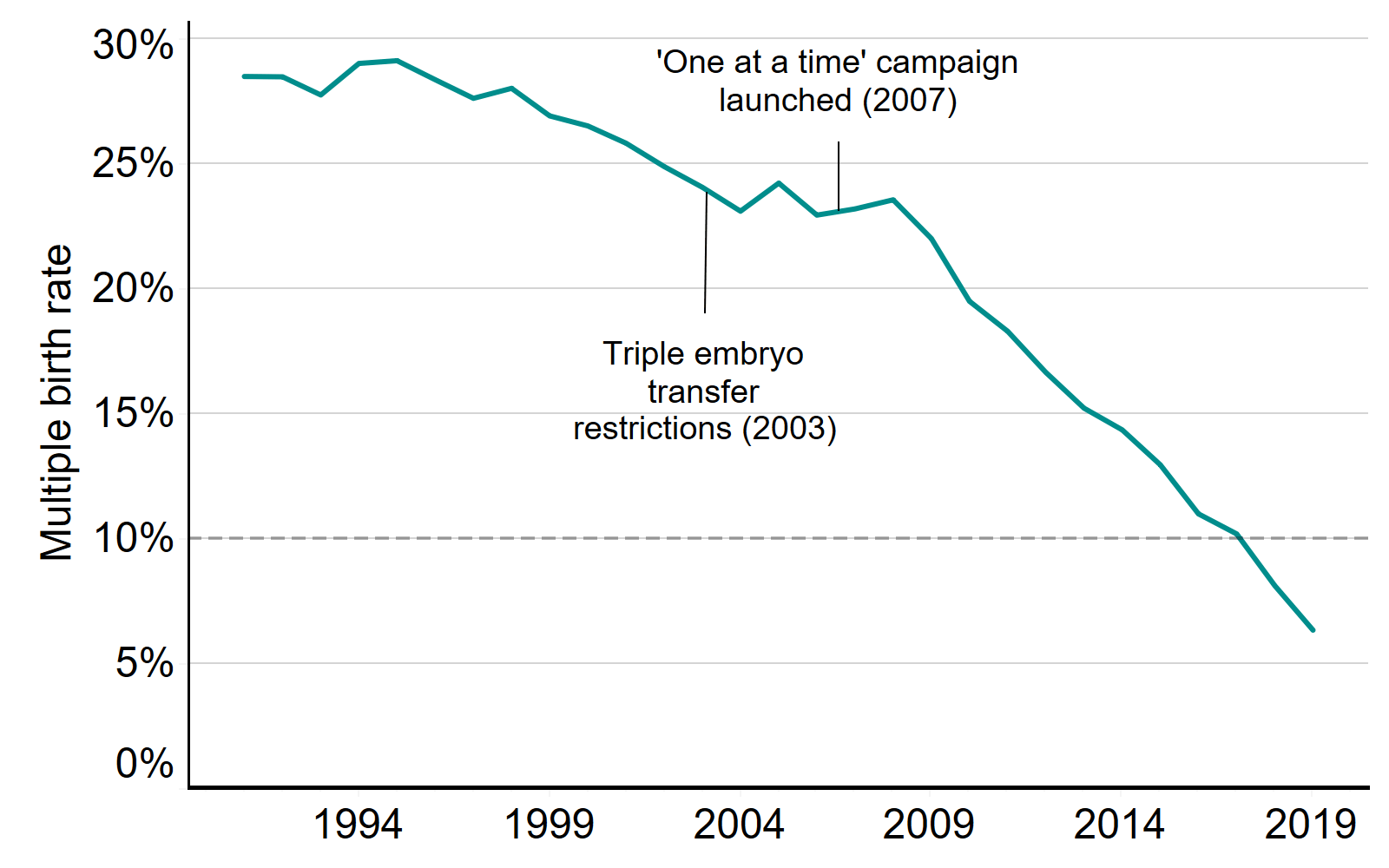
Note figure 1: This data includes treatment cycles and IVF only. It excludes cycles where a pregnancy was recorded but not an outcome.
Download the underlying data for Figure 1 as Excel Worksheet.
2. Single embryo transfers increased most among young patients
Multiple births in IVF treatment are largely determined by the number of embryos transferred back to the womb (see section 4). Single embryo transfers were used in only 13% of IVF cycles in 1991 and increased to 75% of IVF cycles in 2019 (see Fertility treatment 2019: trends and figures).
Following the launch of the ‘One at a time’ campaign in 2007 the use of single embryo transfers greatly increased for all age groups (Figure 2). Single embryo transfers increased most for patients aged 18-35 from 13% use in 2007 to 83% use in 2019.
The larger increase in single embryo transfers among young patients is likely related to professional guidelines and the requirement for clinics to have multiple birth minimisation strategies. Single embryo transfers are recommended in good prognosis patients which includes patients under 37 (at least in their first two rounds of IVF) or in cases where good quality embryos are available (see the HFEA Code of Practice).
Proportion IVF cycles using single embryo transfers and patient eggs by patient age, 1991-2019
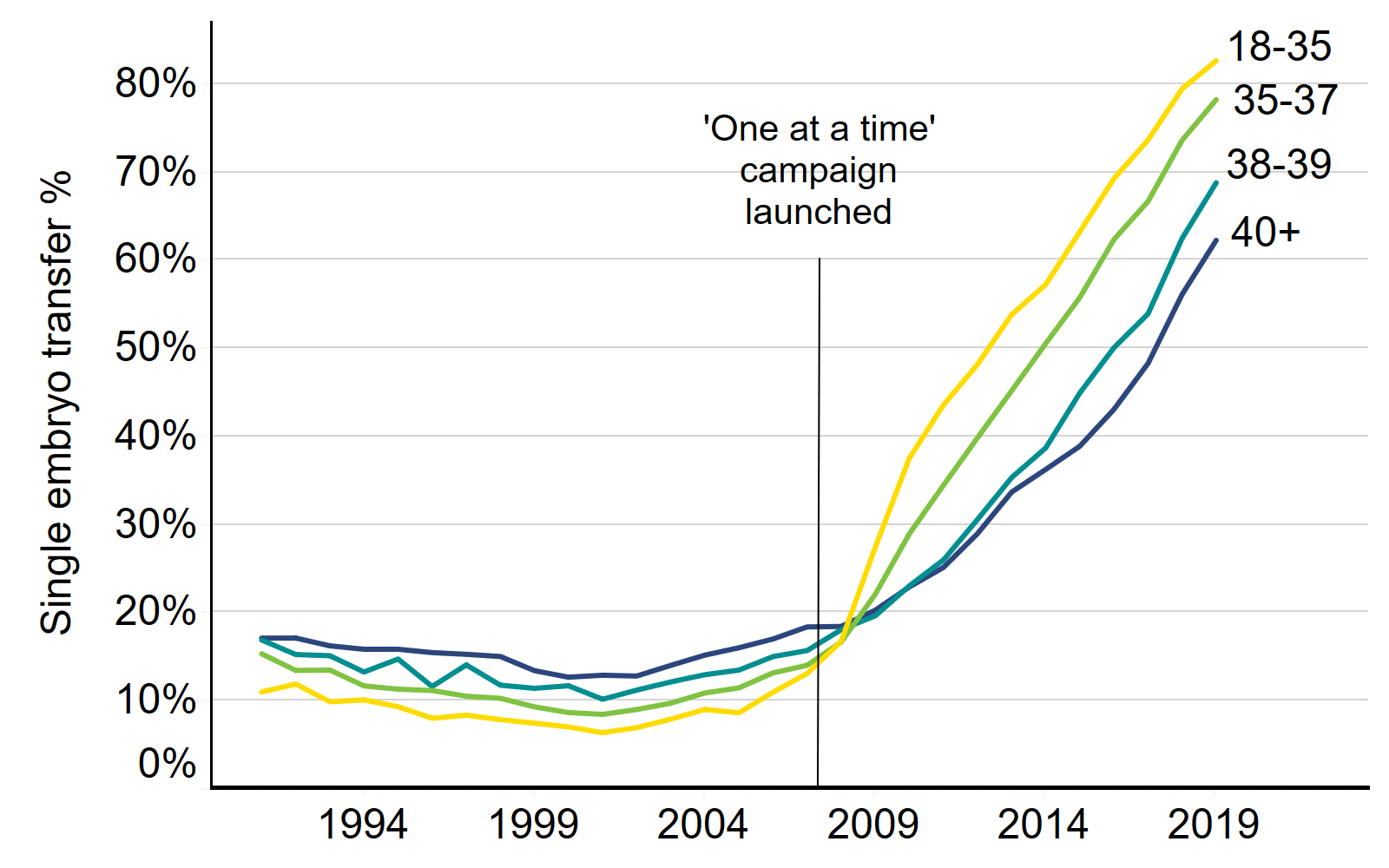
Note figure 2: This data includes treatment cycles and IVF only. It excludes cycles using donor eggs.
Download the underlying data for Figure 2 as Excel Worksheet.
3. Largest improvements in multiple birth rate among youngest and oldest patients
All age groups had an average multiple birth rate under the 10% target in 2019. Figure 3 shows that the multiple birth rate has reduced most among patients aged under 35 (from 27% in 2007 to 6% in 2019) and over 44 (from 31% in 2007 to 5% in 2019).
The decrease in multiple births among patients over 44 is largely due to increased use of single embryo transfers when using donor eggs in treatment, as recommended by professional guidance (see underlying data). Older patients are at a much greater risk of multiple births when using multiple embryo transfers with donor eggs compared to patient eggs (see Section 5). In the early 1990s, only 4% of patients over 44 used single embryo transfers with donor eggs compared to 88% in 2019.
Average live multiple birth rate by age groups, 2007 and 2019
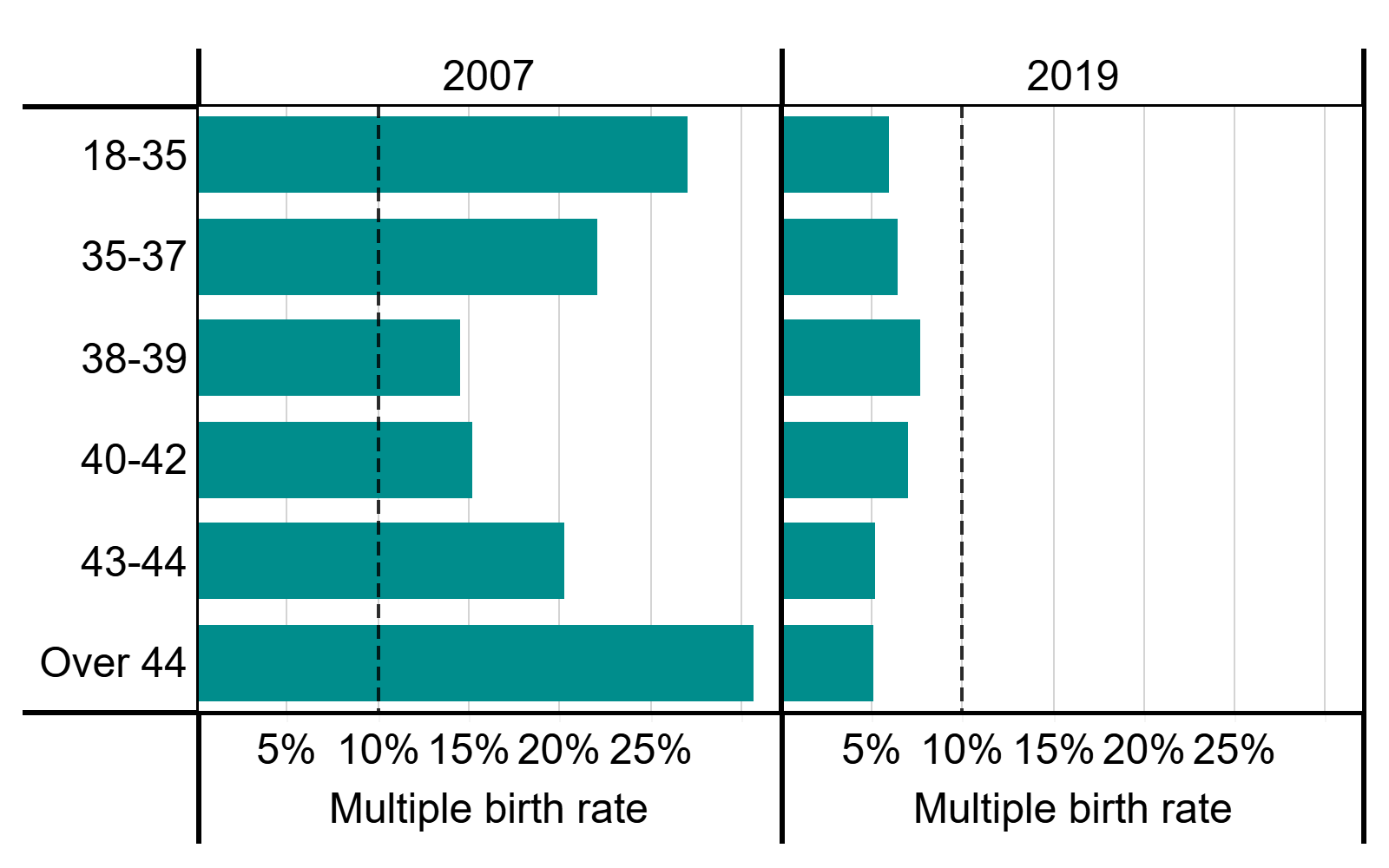
Note figure 3: This data includes treatment cycles and IVF only. It excludes cycles where pregnancy was recorded but not outcome.
Download the underlying data for Figure 3 as Excel Worksheet.
4. Multiple embryo transfers put younger patients at greatest risk of multiple birth
Where patients receive single embryo transfers in their IVF treatment, the average multiple birth rate remains around 1-3% across all patient ages (Figure 4). However, where patients using their own eggs receive double embryo transfers, the multiple birth rate is closely linked to their age, with the highest multiple birth rates (above 30%) recorded for patients aged 35 and under.
Those receiving double embryo transfers are more likely to be poorer prognosis patients (eg. no high quality embryos available or on later IVF cycles) due to recommendations in professional guidance. As the data shown in Figure 4 is an average of those receiving double embryo transfer, it should be noted that individual risk of multiples may be higher among good prognosis patients.
Multiple birth rates decline with age only in cases where the patients’ own eggs are used in treatment. See section 5 for information on multiple birth rates by age when using donor eggs.
Professional guidelines advise that clinics recommend single embryo transfer for good prognosis patients (eg. patients under 37) 5-6. However, in 2019 almost 20% of patients under 37 received double embryo transfers, putting the patient and babies at increased risk of adverse outcomes.
Average live multiple birth rate using patients own eggs by patient age and embryos transferred, 2015-2019
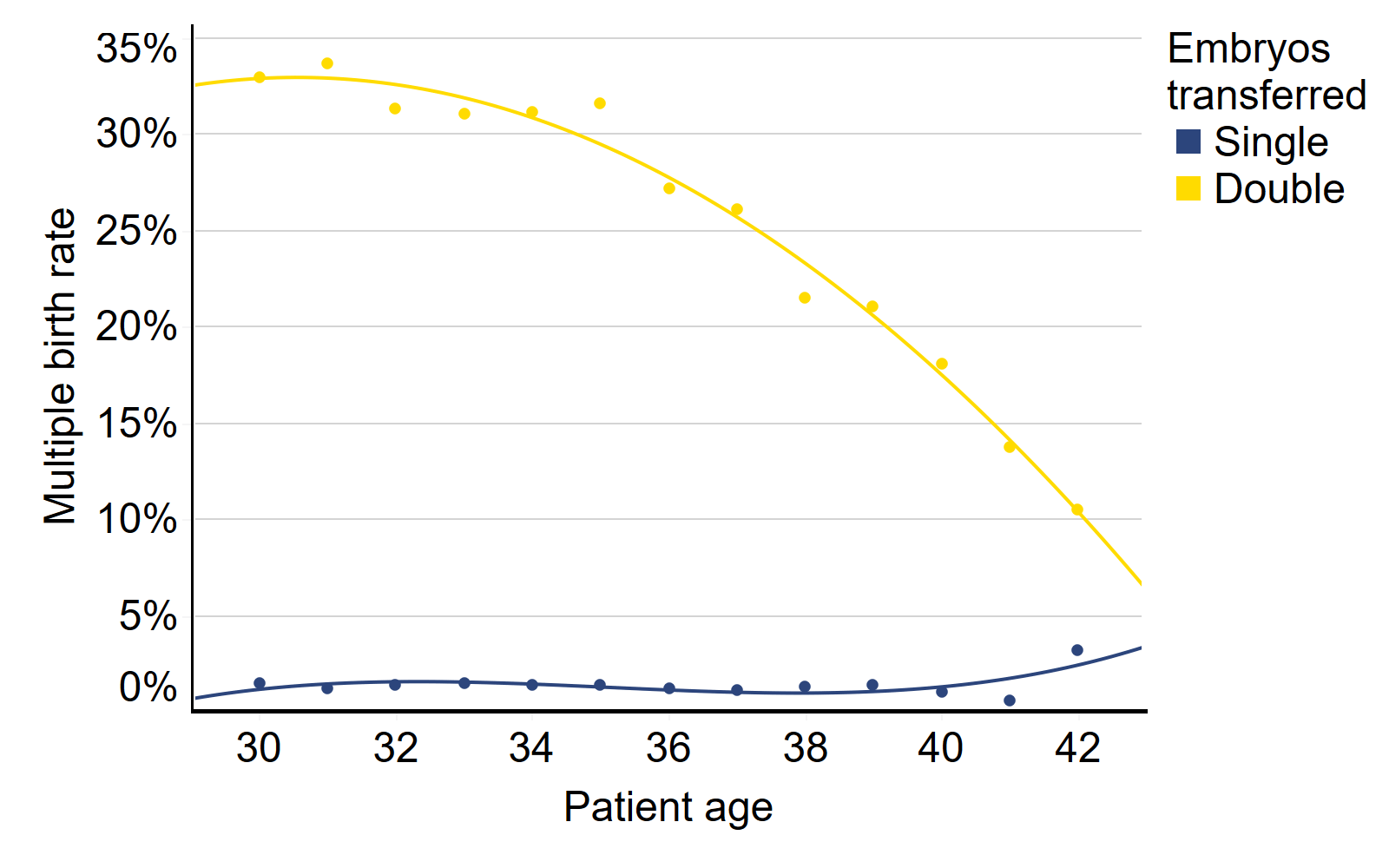
Note figure 4: This data includes treatment cycles and IVF only. It excludes cycles using donor eggs and cycles where pregnancy was recorded but not outcome. Lines included in the graph are lines of best fit and circles represent the average multiple birth rate at individual patient ages. Data presented is on average, multiple birth rates may be higher when using two high quality embryos.
Download the underlying data for Figure 4 as Excel Worksheet.
5. Greater risk of multiple births when using donor eggs
The risk of multiple birth declines with age in IVF treatments using double embryo transfer and patients own eggs. When using donor eggs, the risk of multiple birth can be much greater across all patient ages and this should be considered when making decisions around multiple embryo transfers.
When using double embryo transfers, the multiple birth rate was highest for patients under 35 at over 30% from 2015-2019 and this declined with age to below 15% for patients over 44 (Figure 5), see section 4 for further details on using patients’ eggs. When using donor eggs, the multiple birth rate remained around 30% across all patient ages when using double embryo transfers.
As recommended by the professional guidance, IVF cycles using donor eggs now commonly use single embryo transfers. In 1991, 90% of donor egg IVF cycles used multiple embryo transfers, compared to about 10% in 2019. This has particularly reduced multiple births among patients over 44 (see section 3).
When using donor eggs, the chance of pregnancy is largely dependent on the egg donors age rather than the patients (see Fertility treatment 2019: trends and figures). The risk of having a multiple birth can be higher when using donors eggs because egg donors are typically younger (average age of 30) than the IVF patients using them (35) and egg donors likely do not have known fertility issues.
Average live multiple birth rate from double embryo transfers by age and egg source, 2015-2019
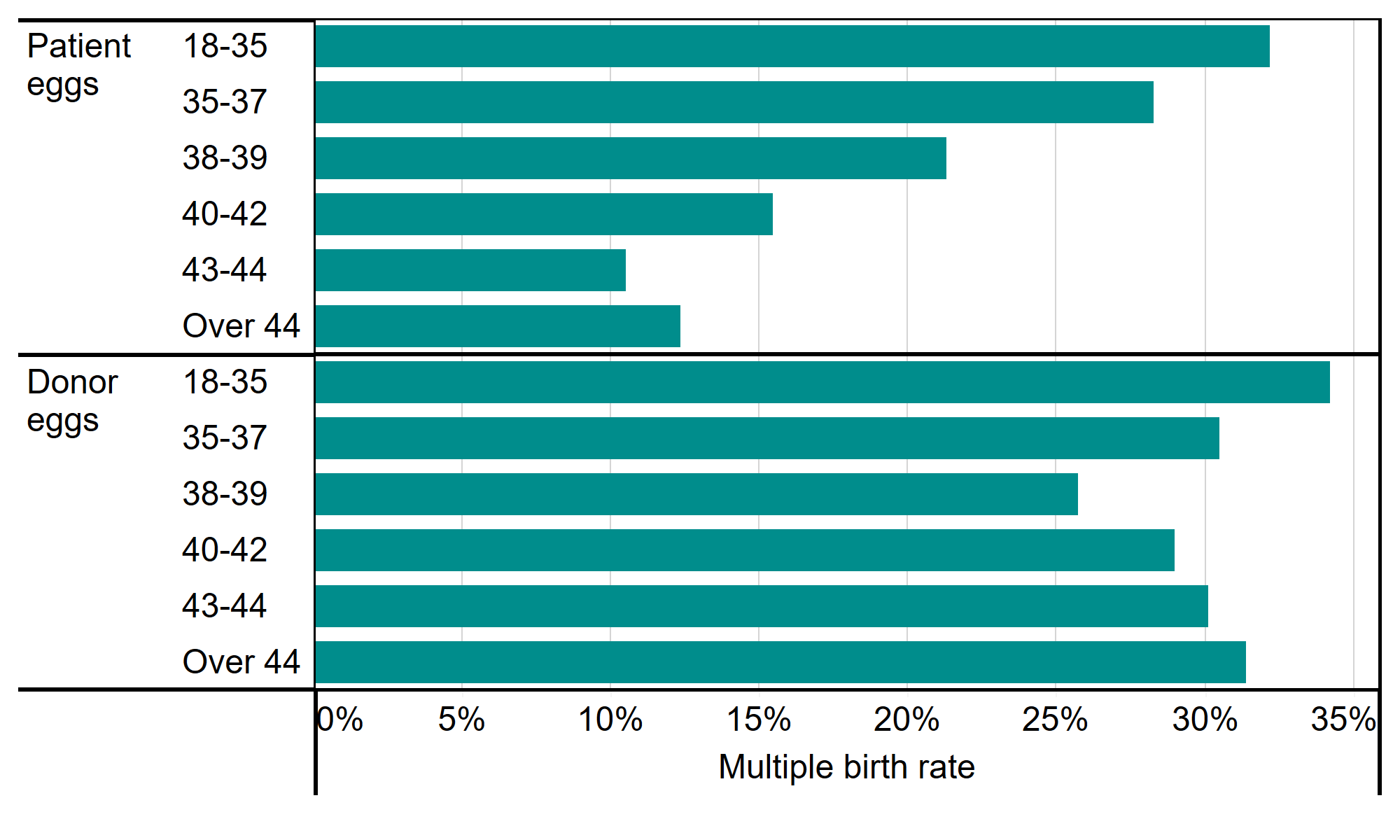
Note figure 5: This data includes treatment cycles and IVF only. It excludes cycles where pregnancy was recorded but not outcome. Data presented is on average, multiple birth rates may be higher when using two high quality embryos.
Download the underlying data for Figure 5 as Excel Worksheet.
6. Multiple birth rates higher among Black patients
In our Ethnic diversity in fertility treatment report 2018, we looked at how fertility treatment use and outcomes varied by ethnic group in the UK. It was found that multiple births were more common among Black patients than other ethnic groups, as were multiple embryo transfers.
The average multiple birth rate using updated 2015-2019 was 10%. White patients had multiple birth rates at 9% which was lower than Black patients at 12%, Other patients at 11% and Asian patients at 10% (Figure 6). Mixed ethnicity patients had a multiple birth rate of 9%.
These variations likely relate to use of multiple embryo transfers in clinical practice. Clinics should be particularly mindful of the higher multiple birth rate among Black patients and seriously consider reviewing their multiple birth policy where necessary.
Average live multiple birth rate by patient ethnicity, 2015-2019
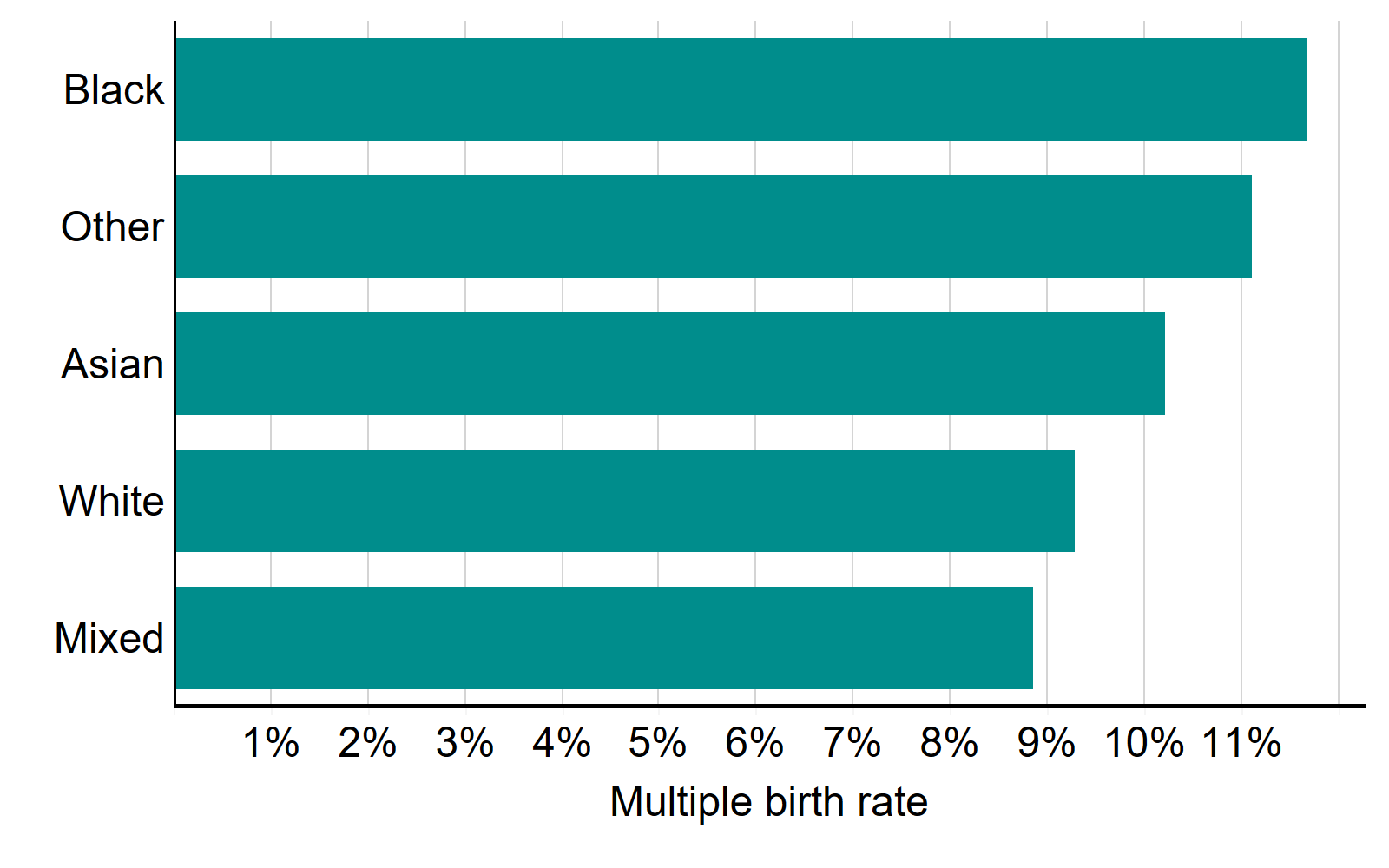
Note figure 6: Cycles where a pregnancy was recorded but not the outcome have been excluded. Full data with 95% confidence intervals available in the underlying figure data.
Download the underlying data for Figure 6 as Excel Worksheet.
7. Higher multiple birth rate among young privately funded patients
The 10% multiple birth rate target has been reached for patients regardless of funding type, with some variation depending on patient age. From 2015-2019, privately funded patients 37 and under had higher rates of multiple births in their first IVF cycle compared to those who were NHS-funded (Figure 7).
The multiple birth rate for patients aged 18-34 was 5% for NHS-funded patients and 9% for privately funded patients from 2015-2019. For patients aged 35-37, NHS-funded patients had an average multiple birth rate of 6% compared to 10% for privately funded patients.
Professional guidelines recommend that all patients under 37 on their first IVF cycle receive single embryo transfer, regardless of available embryo quality. From 2015-2019, patients aged 37 and under on their first IVF cycle more commonly had single embryo transfers when funded through the NHS (81%) compared to those using private funding (72%).
Importantly, there was no difference in birth rate between patients funded by the NHS or those using private funding (see underlying data).
The higher multiple birth rates among young patients may be due to cost related reasons. In Belgium and Quebec, Canada, it was found that improved funding provision, coupled with restrictions on double embryo transfers, reduced multiple birth rates without impacting birth rates 7-8.
Average multiple birth rate on first IVF cycle by funding and patient age, 2015-2019
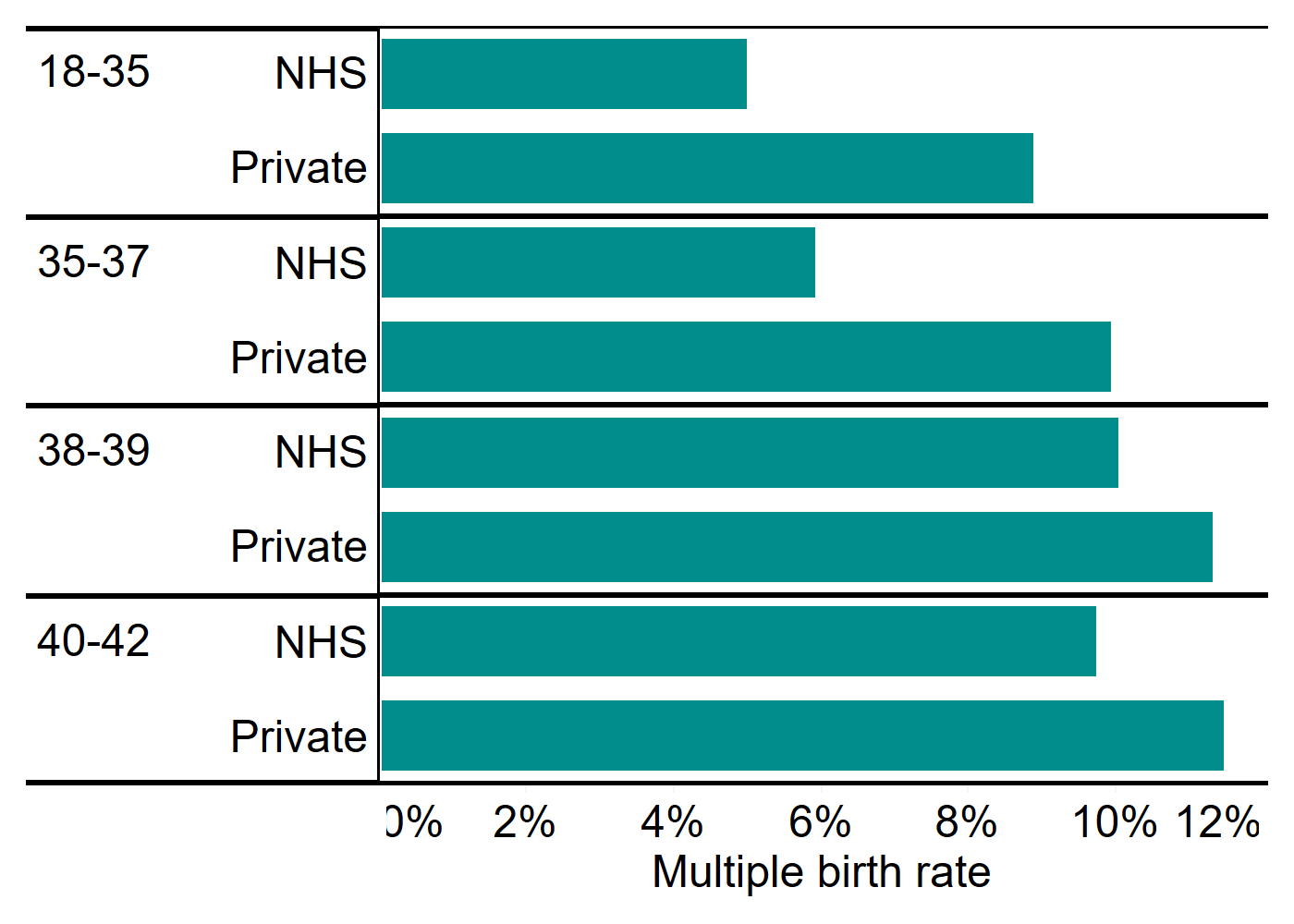
Note figure 7: Data excludes cycles using donor eggs, PGT-A, PGT-M, surrogacy cycles and cycles where a pregnancy was recorded but not the outcome have been excluded. Patients over 42 were excluded due to low NHS funding numbers that make it difficult to compare groups. Full data with 95% confidence intervals available in the underlying figure data.
Download the underlying data for Figure 7 as Excel Worksheet.
8. Twin births risk premature birth and associated health risks
Multiple births increase the health risk of babies born through IVF. Twins are more commonly born premature and underweight, which can lead to long-term health problems such as difficulty breathing, cerebral palsy and other physical and learning difficulties 1-3.
From 2015-2019, about 60% of IVF twin births were born preterm (under 37 weeks) compared to just 9% of singleton births (Figure 8). The health risks are higher the earlier the baby is born. Very preterm births (under 32 weeks) accounted for almost 10% of IVF twins births compared to just 2% for singleton births (underlying data).
Percent of IVF live births born preterm or at term by singleton and twin births, 2015-2019
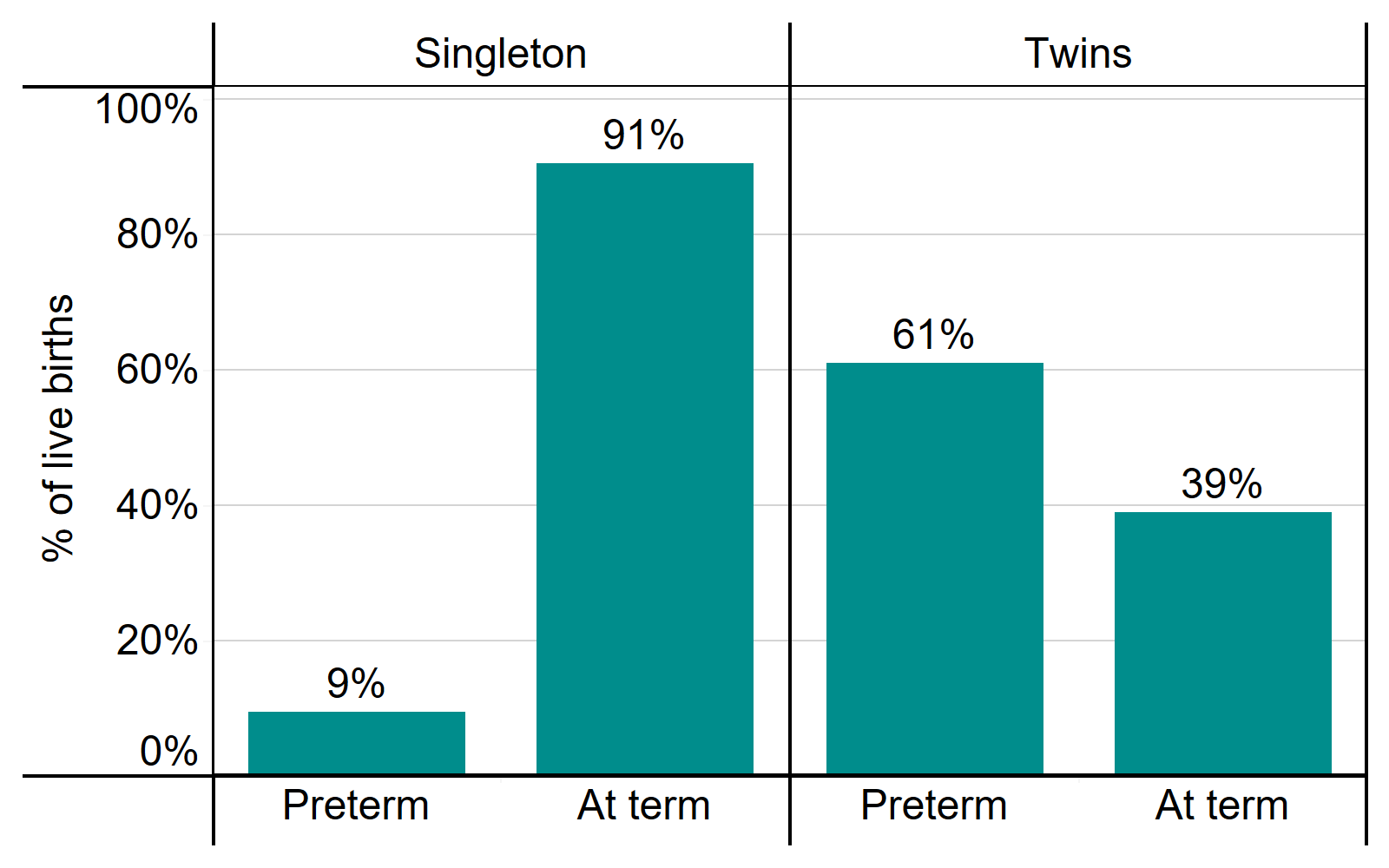
Note figure 8: This data includes treatment cycles and IVF only. It excludes cycles where gestational weeks were not recorded.
Download the underlying data for Figure 8 as Excel Worksheet.
Conclusions and next steps
This report has outlined areas of success in reducing multiple births in fertility treatment following a collaborative approach to drive policy changes with UK professional bodies and concerted efforts across the UK fertility sector. The report also points to areas in treatment where patients and babies may be put at unnecessary risk of multiple births. We are committed to using the data we collect and feedback from our licensed clinics and patients to continue monitoring multiple births in clinics and nationally in the UK, advising on changes where necessary.
In the short term, we will do the following:
- Actions for the HFEA
- We will continue to monitor clinics multiple birth rates on inspection and encourage clinics to review their minimisation strategies in relation to patients from ethnic minority groups.
- We will continue to work with clinics that are non-compliant with the 10% target to improve their minimisation strategies through inspections (further details in State of the Sector).
- We will continue to monitor multiple birth rates nationally and provide annual updates in Fertility treatment: trends and figures.
- We will open a dialogue with professional bodies, patients and clinics, with the aim of considering a future review of the 10% multiple births limit.
- We carried out a national patient survey with questions on multiple birth decision making in November 2021. The results from this survey will be published on our research and data page in May 2022.
- Actions for clinics
- We urge clinics to review their own information provision in relation to the statistics in this report to ensure all patients are informed of their own likely chance of multiple birth based on all factors, including age and donor egg use.
- Clinics should be mindful of the higher multiple birth rate in certain ethnic groups and seriously consider a review of their multiple birth minimisation strategies where necessary.
- Actions for others
- We continue to encourage all those who commission fertility services to review their funding provision in line with NICE recommendations and consider whether their policy has an adverse impact on multiple births.
- This report is limited by the data we hold on our Register and more research is needed to understand the many external factors that contribute to decisions around multiple embryo transfers. We have an anonymised register of cycle level data that is publicly available on our website for research purposes which includes number of embryos transferred and birth outcome information.
- More in-depth data is available to researchers upon application through the HFEA Register Research Panel and we encourage researchers to get into contact with us at register.research@hfea.gov.uk if interested.
We are committed to reducing the health risks posed by multiple births due to fertility treatment in the UK. We will continue to report this information to monitor actions in this area.
About our data
The information that we publish is a snapshot of data provided to us by licensed clinics. The figures supplied in this report are from our data warehouse containing Register data as at 12/12/2020. We have excluded approximately 1,540 cycles due to technical issues at one centre that resulted in reporting errors. Results are published according to the year in which the cycle was started. Due to rounding, some percentages may not add to 100%.
Assisted reproductive technologies are a rapidly evolving field and practices such as number of embryos transferred and NHS funding have changed over this time – these changes are documented in Fertility Trends. For this report, where numbers were small in a single year, we have compiled up to five years of data to provide more robust estimates for comparison.
Our live birth data counts all births where one or more babies were born showing some sign of life, including those who go on to die within the first month of life (neonatal deaths). Our multiple birth data counts only births where two or more babies were born alive, including those where one or more of the babies die within the first month of life. Multiple birth rates provided throughout the report are averages across the UK for IVF treatment only, see underlying data for DI multiple birth information.
For further information, please see our quality and methodology report and information page in the underlying dataset.
Contact us regarding this publication
Media: press.office@hfea.gov.uk
Statistical: intelligenceteam@hfea.gov.uk
Accessibility: comms@hfea.gov.uk
Notes on Multiple births in fertility treatment 2019
- IVF Risk by National Health Service
- Perinatal outcomes in twin pregnancies complicated by maternal morbidity: evidence from the WHO Multicountry Survey on Maternal and Newborn Health, BMC, 2018, 18: 449
- What Are the Fetal Growth Patterns of Singletons, Twins, and Triplets in the United States?, Clinical Obstetrics and Gynecology, 1998, 41: 115-125.
- Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Death and Morbidity 2015-2017 by Mothers and Babies: reducing Risk through Audits and Confidential Enquiries across the UK
- Guidance on number of embryos transferred by the National Institute for Health and Care Excellence
- Code of practice 9th edition by the HFEA
- The impact of legally restricted embryo transfer and reimbursement policy on cumulative delivery rate after treatment with assisted reproduction technology, Human Reproduction, 2014, 29: 267-275.
- Universal coverage of IVF pays off, Human Reproduction, 2014, 29: 1313-1319.
| Publication date: |
|---|

