Egg donation: a factsheet
A statement from the HFEA.
Clare Ettinghausen, Director of Strategy and Corporate Affairs, said:
“There is a lot of information about egg donation and the recent increase in donor compensation. As the UK’s fertility regulator, we want to ensure that people are receiving correct information in the interest of patient safety and clarity.
“About 1 in 153 of all children now born in the UK are conceived through donation of egg or sperm. Without a donor, many families wouldn't have been able to have a much-wanted baby.
“Donating eggs and sperm is an amazing altruistic act that helps create much longed-for families. However, donating eggs, sperm, or embryos to someone else is a serious commitment with lifelong implications, such as the fact donors must be comfortable that any children born from their donation can find out identifiable information about their donor when they turn 18.
“The process of donating eggs is generally very safe but, like any medical procedure, it carries some risk and takes around three to four weeks to complete. Patient safety is of the utmost importance, donors will go through rigorous medical screening and clinics should do everything possible to prevent and manage Ovarian Hyperstimulation Syndrome (OHSS). In 2024/25, there were 67 cases of severe and critical OHSS reported by UK clinics. None of these cases related to egg donors.
“These FAQs provide accurate and impartial information for anyone either considering becoming a donor or who wants to find out more about the process and reasons behind uplifting compensation amounts. We always urge people to do their research when it comes to anything related to fertility treatment, and the best place to start when finding out factual information is on the HFEA website.”
Ends
1. Egg donation in general
Use of donor eggs, sperm and embryos in fertility treatments has increased over the last decade, accounting for around 1 in 153 of all live births in the UK in recent years.
Egg donation is an altruistic act that helps 2-3,000 people a year who otherwise wouldn’t be able to have a baby. Academic research has found that people donate in the UK for altruistic reasons – often after having some experience of fertility problems through family members or friends.
Choosing to become a donor is a complex decision, with implications for the donor and their wider family, the recipient, and any child born as a result. For example, donors will go through rigorous medical screening and must be comfortable with the fact that any children born from their donation can contact them when they turn 18.
Donors can consent for their eggs or sperm to be stored for use for any period up to 55 years, since a change in the law in July 2022. Previously, people consented for up to ten years.
2. How old are egg donors?
Our data shows that egg donors had a consistent average age of 31-32 from 1991-2020. See the below from the underlying data set of our Trends in egg, sperm and embryo donation 2020 report:
| Donor type and time period | Age 18-25 | Age 26-30 | Age 31-35 | Age 36-40 | Age 41-45 | Age 46-50 | Other or unknown age | Median age |
| Egg donors, 1991-2000 | 736 | 2,203 | 3,683 | 673 | 181 | 92 | 12 | 32 |
| Egg donors, 2001-2010 | 1,100 | 2,781 | 4,893 | 1,591 | 402 | 121 | 37 | 32 |
| Egg donors, 2011-2020 | 2,803 | 4,265 | 5,737 | 1,499 | 380 | 122 | 12 | 31 |
3. What is the socio-economic background of egg donors
Our 2022 report found that egg and sperm donors in England from 2011-2020 lived in similar or more affluent socio-economic areas than the general population. This, in combination with previous academic research, suggests that UK sperm and egg donors largely donate for altruistic reasons.
4. Are they already parents?
Some egg donors already have their own child. In 2020, around 1 in 3 (31%) of egg donors already had their own child.
5. Why is the HFEA encouraging egg donors to come forward?
The HFEA does not advertise for donors. UK licensed clinics are able to recruit donors and should follow the law and guidance set out in our Code of Practice.
This states that “Advertising or publicity aimed at recruiting gamete or embryo donors, or at encouraging donation, should not refer to the possibility of financial gain or similar advantage, although it may refer to compensation permitted under relevant HFEA Directions”.
6. Why is egg donor compensation being raised from £750 to £985?
There has been widespread interest in donation in recent years and our figures show that the number of new egg donors continues to rise. So, earlier this year, our Authority met to discuss the rates of compensation currently being offered to egg and sperm donors. Egg donors will receive £985 and sperm donors will receive £45. The increase in donor compensation later this year will be the first since 2011 and reflects the rise in inflation rather than any intent to monetise donation in the UK.
7. What if I see advertising that concerns me?
Any advertising should be carried out in line with the Advertising Standards Authority codes and the joint enforcement notice for the fertility sector and information for patients in line with our Code of Practice and consumer law.
8. What about the risks?
The process of donating eggs is generally very safe and comparable to patients who undergo IVF but, like any medical procedure, it carries some risk and takes around three to four weeks to complete.
In some very rare cases people develop Ovarian Hyperstimulation Syndrome (OHSS). OHSS is a very serious and potentially fatal reaction to fertility drugs, which happens about a week after your eggs have been collected.
Patient safety is of the utmost importance and we work closely with clinics to do everything possible to prevent and manage Ovarian Hyperstimulation Syndrome (OHSS). In 2024/25, there were 67 cases of severe and critical OHSS reported by UK clinics. None of these cases related to egg donors.
Symptoms include a swollen stomach and stomach pains and, in extreme cases, nausea, vomiting, breathlessness, fainting, a swollen stomach and reduced urine.
If you have any reactions to your fertility drugs, it’s very important you let your clinic know straight away. Never feel like you're wasting their time.
9. Do clinics have to explain the risks to patients?
Yes. Our Code of Practice states that donors must be selected on the basis of their age, health and medical history, provided on a questionnaire and through a personal interview performed by a qualified and trained healthcare professional.
This assessment is to identify and screen out potential donors whose donations could present a health risk to others, such as the possibility of transmitting diseases, or health risks to themselves, including superovulation, sedation or the risks associated with the egg collection procedure or the psychological consequences of being a donor.
10. What is the process?
The process for donating is exactly the same as the early stages of IVF and takes around 2-3 months from initial contact with a clinic to the egg collection. Each clinic will have their own medication protocol to get you ready for egg collection. An example of how this may be done is below:
- Usually, you will start hormone treatment on day 2 of your cycle. This involves taking a daily injection of follicle stimulating hormone (FSH) to boost the number of follicles (which may contain eggs) your body usually produces.
- After a few days you will start another daily injection (an antagonist) to suppress your natural hormone production.
- You will need to have either blood tests, scans or sometimes both, to check your response to the medication. You may need to have several visits to your clinic.
- When your follicles reach a certain size, you will be ready to be given an injection to help the eggs mature (an agonist).
Your eggs will be collected while having pain relief. Sometimes you may be sedated or under general anaesthetic. The procedure takes around half an hour.
It’s worth bearing in mind that, even when the donation is complete, donors have the right to withdraw or vary their consent up to when the embryos are transferred to a patient.
11. Why do people import donor eggs?
Egg donors are typically UK donors, with only around 3% imported from abroad. One reason that patients may import donor sperm or eggs is to find a donor of matching ethnicity. This is backed up by our 2021 National Patient Survey, which found that 82% of respondents said it was important that the ethnicity of a donor matched their own.
In our Ethnic Diversity in Fertility Treatment report, we found that while most donor eggs used were from the UK, donations from donors of Other ethnicities were most likely to be imported (7%) followed by Black and Asian donors (3%) – see Figure 4 of the report below.
There are many more egg donors in the UK from white backgrounds than from Black, Asian or other ethnic groups e.g. in 2023 there were around 55 new Black egg donors, 60 Asian, and 1,070 White.
Figure 4: Over half of Mixed, Other and Black donor sperm used in IVF treatments were imported from abroad
Proportion of IVF cycles using imported donor sperm and eggs by donor’s ethnicity, 2017-21 (preliminary 2020-21 data)
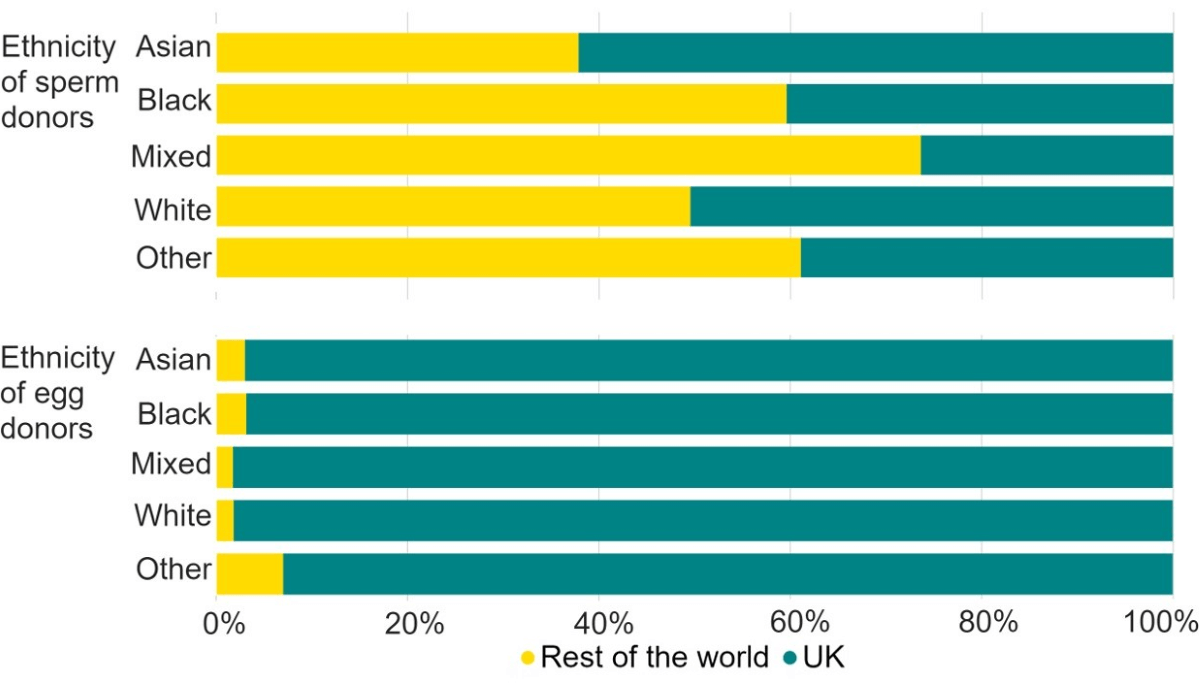
Note figure 4: Data for 2020 and 2021 is preliminary and has not been validated. This data excludes DI cycles and includes IVF treatment cycles begun with the intention of immediate treatment, instead of storing eggs or embryos for future use.
12. Is there a shortage of eggs?
Our recently published Fertility Trends report show that the number of egg donors continues to rise in the UK. However, we also know that in some parts of the UK there are long wait times, particularly where there are patients struggling to find donors that meet their requirements, such as ethnicity.
We’d always recommend patients use our Choose a Fertility Clinic tool to find out approximate wait times, but would strongly advise they contact clinics directly as well, as they will be able to provide more in depth information and specifics.
13. Fertility treatment abroad
We don’t have any data on the numbers of people going abroad, but we know that some patients are attracted by the offer of cheaper treatment abroad, finding a donor with a similar ethnic background or shorter waiting times for donor treatments. Fertility treatment isn’t regulated in other countries in the same way as it is in the UK. We would therefore encourage anyone thinking of going abroad to read the information on our website.
14. Links to our information and reports on donation
Using donated eggs, sperm or embryos in treatment
Family formations in fertility treatment 2018
Trends in egg, sperm and embryo donation 2020
Ethnic diversity in fertility treatment 2021
Fertility treatment 2023: trends and figures
Fertility treatment for LGBT+ people
Authority (Board) paper on the decision to increase compensation.
| Publication date: |
|---|

