Breaking the myths about Endometriosis
By Emma Cox, Chief Executive, Endometriosis UK
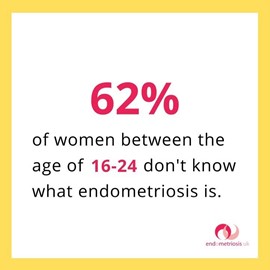
March is Endometriosis Awareness Month, and awareness of this chronic and often misunderstood disease is very much needed. Endometriosis, a leading cause of infertility, affects 10% of women and those assigned female at birth, and its most common symptom is chronic, sometimes debilitating, pelvic pain. Despite affecting so many, few have heard of it: 62% of 16-24-year-old women don’t know what it is, nor have 75% of men of all ages.
It takes, on average, 8 years to get a diagnosis of endometriosis, a shocking length of time that hasn’t changed in over a decade. The impact of delayed diagnosis on people’s physical and mental health can’t be overstated. If undiagnosed, treatment cannot be accessed and the disease may progress, and negatively impact people’s careers, education, relationships, and all aspects of their life.
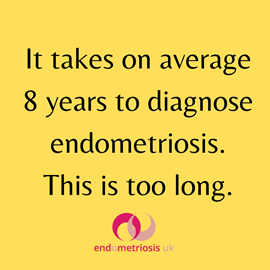
A combination of factors contribute to such lengthy diagnosis times. Our research shows that 80% of women aged 16-24 would put off going to the Doctor with symptoms of endometriosis. Lack of education about menstrual wellbeing means those suffering symptoms such as chronic pelvic pain may thing it’s what everyone experiences. There can be embarrassment or cultural taboos around discussing menstrual issues, and when help is sought, healthcare practitioners may not recognise the symptoms, nor believe the severity. Pelvic pain may be normalised, claimed to be due to ‘a low pain threshold’ or ‘all in your head’. Prior to a diagnosis, due to their symptoms, 58% go to the GP over 10 times, and 43% had five or more hospital visits – all before endometriosis was even mentioned as a possibility.
The message is this is something you have to put up with, and it’s not serious. However, pelvic pain so severe it interferes with your everyday life is not normal, and those experiencing it deserve to be listened to and treated seriously as they should any medical condition. Just because it’s linked to the menstrual cycle and periods shouldn’t mean it’s less important.
One of the commonest stories we hear is about an adolescent or young woman going to the doctor with severe pelvic pain, and being ‘put on the pill’ with no explanation sought as to what is causing the pain. Why are we medicating sometimes very young people without looking for the cause? By not diagnosing endometriosis, we are denying the opportunity for an individual to make choices about their future, especially around their fertility. Access to fertility preservation is also an issue, with women as young as in their late teens being told their only chance of a biological family in the future is fertility preservation, which they do not have the means to access.
Whilst many with endometriosis will be able to get pregnant naturally, it does increase the risk of infertility. Hormonal treatments, such as the contraceptive pill or a medically induced menopause may help manage the symptoms for some, but aren’t an option if fertility is a priority.
There are myths we must overcome if diagnosis times are to be driven down. Severe period pain is not ‘normal’; those experiencing severe period pains do not have ‘a low pain threshold’, and one of the most dangerous: the myth that pregnancy can cure endometriosis (it doesn’t). It is wrong that pregnancy is recommended as a ‘treatment’.
This Endometriosis Awareness Month, Endometriosis UK is calling an end to the stigma associated with endometriosis, and is asking:
- UK Governments to make a commitment to reduce diagnosis time for endometriosis with a target of an average of 4 years or less by 2025, and a year or less by 2030.
- To ensure a minimum baseline for endometriosis diagnosis, treatment and management is available to all those who need it, not a postcode lottery, by implementing the NICE Guideline on Endometriosis Treatment and Management (2017), adopted by the NHS’s across the UK but not implemented.
- A commitment from all 4 nations to include compulsory menstrual wellbeing in the school curriculum so that young people recognise the warning signs of menstrual health conditions and know when to seek help. This is compulsory in schools in England from 2020, but is not UK-wide.
- Employers to recognise the impact of endometriosis in the workplace and afford their colleagues the support they need to manage their condition, as they would any other chronic condition.
- For anyone experiencing any of the symptoms of endometriosis to recognise they may need help and be confident to contact their GP, not be put off by stigmas associated with the condition or delay seeking advice due to the COVID-19 pandemic. Symptoms include: chronic pelvic pain, painful periods, painful sex, painful bowel movements, difficulty getting pregnant, fatigue.
For more information about endometriosis, visit Endometriosis UK’s website.
About the author: Emma joined Endometriosis UK as Chief Executive in February 2016, and has overseen a sustained period of growth and development for the organisation, including awareness raising, new campaigns, and building key relationships with healthcare practitioners, researchers and policy influencers.
Emma’s background is as strategic change management specialist with over 20 years’ experience gained working in volunteering, membership organisations including Diabetes UK, NUS and the Chartered Quality Institute. Emma has an MSc in Organisational Behaviour and an MBA.